Central sensitization is a condition of the nervous system thought to be associated with the development of chronic pain conditions. Central sensitization occurs when the nervous system becomes “up-regulated” to be in a persistent state of high reactivity. The progression toward an up-regulated nervous system usually begins long before a central sensitization condition manifests. After an injury, the continual state of nervous system activation maintains pain even though the initial injury may have healed.
Central sensitization involves a heightened sensitivity to pain and a heightened sensitivity to the sensation of touch. Because the nervous system is in a persistent state of heightened reactivity, the sensation is registered in the brain as painful when it normally wouldn’t be. People with chronic pain can experience pain with a simple touch of the hand. Or, when a painful stimulus occurs, the sensation of pain is registered in the brain as more intense than it normally would be.
Central sensitization can also lead to heightened sensitivities across all senses, not just the sense of touch. People with chronic pain can sometimes report sensitivities to light, sounds and odours. Central sensitization is also associated with cognitive changes, such as poor concentration and poor short-term memory. It is typically accompanied by increased levels of emotional distress, particularly anxiety. The nervous system is in a persistent state of reactivity, so people feel ‘nervous’ or anxious. Lastly, central sensitization is also associated with a change in behaviours around this constant challenge. People with chronic pain can often be seen to be resting, feeling sick, avoiding otherwise normal experiences or stimuli and adopting a new “sickness” identity in their lives. It is common for people with chronic pain to feel “crazy” because they are experiencing sensations other people aren’t. Sometimes it’s their friends and loved ones who begin to wonder if the person with chronic pain is a hypochondriac or just exaggerating. Sadly, this can lead to strained relationships, job failure, lack of social support, and ultimately isolation and loneliness. Often the stress of loneliness can exacerbate the central sensitization condition.
Cause of Central Sensitization
Research has shown increasingly that central sensitization plays a role in many different chronic pain and chronic illness disorders. It can occur with chronic low back pain, chronic neck pain, whiplash injuries, chronic tension headaches, migraine headaches, rheumatoid arthritis, osteoarthritis, endometriosis, motor vehicle accident injuries, and post- surgical pain. Fibromyalgia, irritable bowel syndrome and chronic fatigue syndrome all seem to have the link to central sensitization as well.
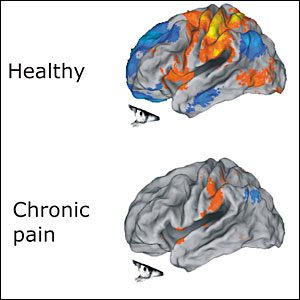
Central sensitization involves specific changes to the nervous system. Changes occur at the cellular level in the brain and in the central nervous system. Injuries to the central nervous system, such as stroke or spinal cord injuries have been shown to cause central sensitization. More recently, studies have linked more common pain experiences such as headache or low back pain to central sensitization as well.
Central Sensitivity Syndrome is the diagnosis given to someone withr a condition of central sensitization. It is likely caused by multiple factors. A person suffering with chronic pain likely had significant pre-disposing factors at play which heightened the reactivity of their central nervous systems before the onset of central sensitization occurred. These prior conditions can be biological, psychological and environmental. If the nervous system is reactive prior to injury, then the nervous system might be more prone to central sensitization once onset of pain occurs. Low and high sensitivity to pain are likely due at least in part to multiple genetic factors, as are general sensory sensitivities, and anxiety and stress regulation. Stress responses as well as anxious thinking are linked to higher subjective experiences of chronic pain in the research. These psychophysiological factors suggest that the pre-existing state of the nervous system is an important determinant of developing central sensitization. A prior history of anxiety, physical and psychological trauma, and depression are significantly predictive of onset of chronic pain later in life. They are all conditions of the nervous system, particularly a persistently altered, or dysregulated, nervous system. The already dysregulated nervous system, at the time of injury, may interfere with the normal trajectory of healing and thereby prevent pain from subsiding once tissue damage heals.
There are also factors that occur after an injury has occurred which can play a role in the development of central sensitization. It is a common response with the onset of pain to experience depression, fear-avoidance, anxiety and negative interpretations of pain. These responses, as well as changes in sleep and self-care patterns, which are a common consequences of living with chronic pain, can, in turn, further exacerbate the reactivity of the nervous system, leading to central sensitization.
Treatments of Central Sensitivity Syndrome
Treatments for chronic pain syndromes that involve central sensitization typically target the central nervous system or the inflammation that corresponds with central sensitization. Medical treatments involve anti-depressants, anti-convulsant and anti-inflammatory medications, as well as more invasive treatments to physically block nerve signals. Psychological treatments include cognitive behavioural therapy to reduce anxiety and change behaviours that maintain pain states.
At Stillwater Counselling, Megan Hughes targets underlying trauma states in order to reduce the hyper-arousal of the nervous system. She utilizes EMDR to desensitize and process traumas held in the body. Then, using Cognitive Behaviour Therapy, as well as clinical hypnosis and relaxation and breathing exercises, Megan Hughes helps clients with chronic pain and chronic illness to learn to regulate their nervous systems and manage their sensitivities. An important part of self-regulation is learning how to self-care differently. Movement is recommended to people with chronic pain and chronic illness in order to reduce the effects of central sensitization and to avoid engaging in a negative pain cycle.
[Adapted from the Institute for Chronic Pain]